Is The Affordable Care Act Working?
The Affordable Care Act (ACA) was meant to usher in a new era of healthcare, insuring millions more Americans and improving health care access. While the current state of The Affordable Care Act is still under scrutiny as it once again faces legal hurdles after President Donald Trump and his administration supported a lawsuit questioning the health-care law’s constitutionality, it’s important to ask the question, is it working?
The original intent of the Affordable Care Act was to protect patients while simplifying the system for buying health insurance and paying healthcare providers. It planned to accomplish this with 3 main objectives: (1) to reform the private insurance market, especially for individuals and small-group insurance purchasers, (2) expand Medicaid to the working poor with income up to 133% of the federal poverty level, and (3) to change the way that medical decisions are made.
In 2010, the House and Senate under Democratic control passed the law and granted healthcare coverage for more than 20 million people. The law included a provision requiring all those who could afford it to have basic insurance or pay a tax, or in other words, a penalty.
In 2012, the Supreme Court upheld the law in a 5-4 decision when Chief Justice John G. Roberts Jr. said the tax penalty was constitutional because it was not a “legal command” but gave people a choice: Buy insurance or pay a tax.
However, in 2016, Donald Trump won the election after promising repeatedly to “repeal and replace” Obamacare. Though Republicans controlled the House and Senate, they did not repeal the law. Instead, in July of 2017, one repeal effort famously failed when GOP Sen. John McCain walked on to the Senate floor and gave a thumbs-down signal.
In 2018, Texas Atty. Gen. Ken Paxton joined with 20 other states to file a new suit in a federal court in Fort Worth seeking again to strike down the law.
Congress meant for the individual mandate to be the centerpiece of Obamacare. Without the constitutional justification for the centerpiece, the law must go down, Paxton said. Obamacare is a failed social experiment. The sooner it is invalidated, the better.
In December 2018, U.S. District Judge Reed O’Connor agreed with the Texas lawyers and decided the entirety of the law was unconstitutional. And now, Trump administration lawyers decided to go further and argue that the courts should void the law that the Republican Congress was unable to repeal.
So where do we stand with the Affordable Care Act? The intent of the Act, at its’ core was done in good faith. But, does it work?
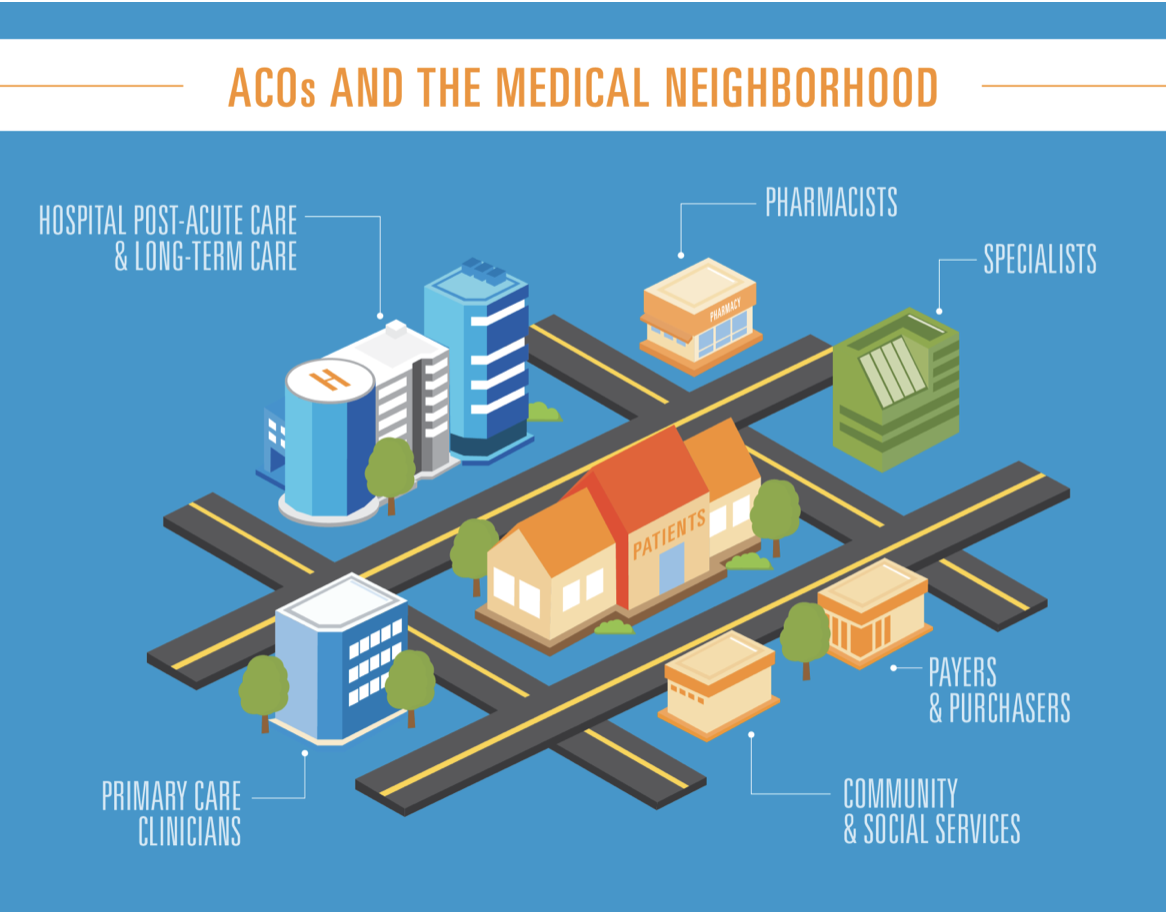
Unfortunately, years after its passage, programs are falling short of expectations. One such area is the Accountable Care Organization (ACO). This program was intended to address the exorbitant costs of Medicare all while significantly improving patients’ quality of care. However, ACOs have not lived up to expectations, and the Centers for Medicare & Medicaid Services (CMS) are putting their foot down by requiring new levels of accountability. It’s time Medicare said enough is enough.
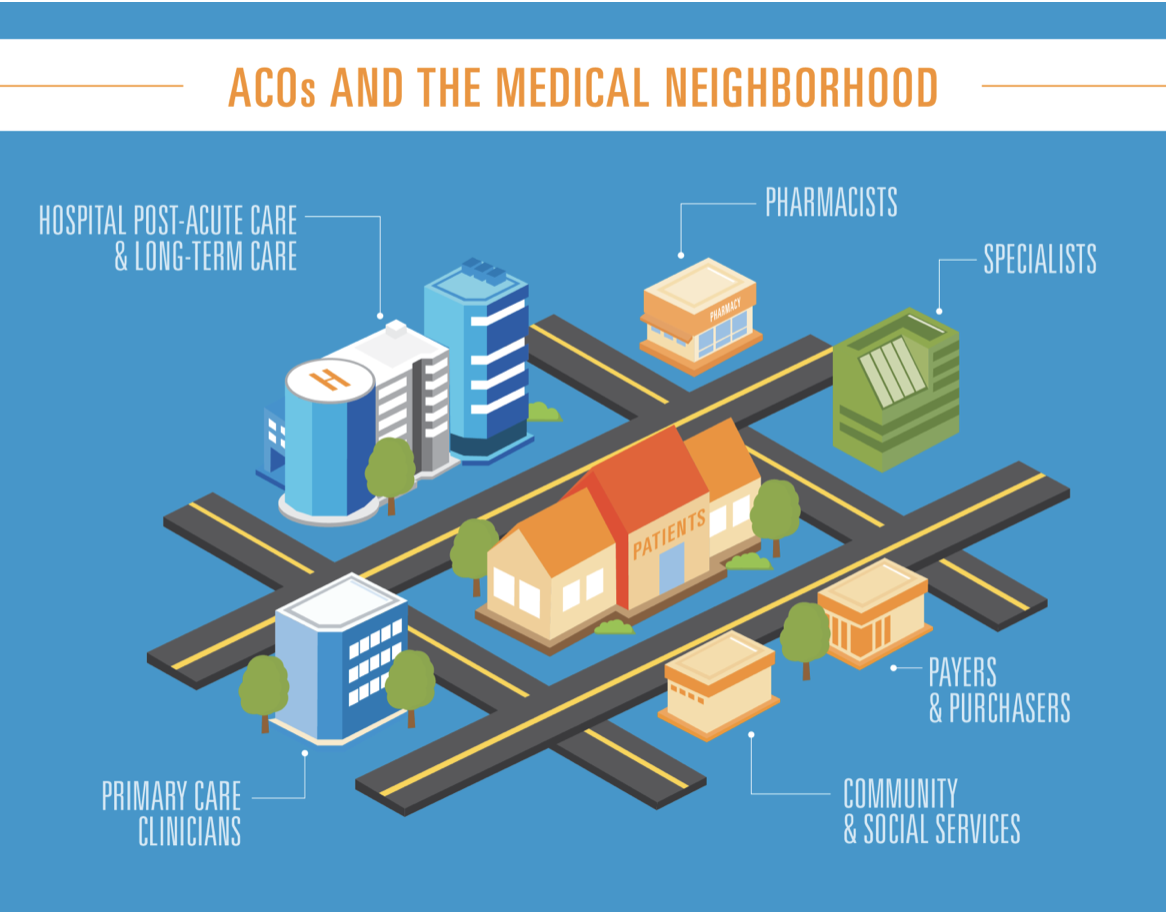
Let’s back up. First, what are Accountable Care Organizations? ACOs are voluntary groups of physicians, hospitals and other healthcare providers that band together to take responsibility for the quality of care for Medicare patients while decreasing costs. These organizations were formed under the ACA Medicare Shared Savings Program. The Shared Savings Program is a voluntary program that encourages groups of doctors, hospitals, and other health care providers to come together as an ACO to give coordinated, high quality care to their Medicare beneficiaries. Its three-part mission is to promote accountability for the patient population, coordinate services for beneficiaries, and encourage investment in high-quality, efficient services. ACOs were supposed to be accountable for quality, cost, and experience of the Medicare beneficiaries while being rewarded by benefits and savings for their organization. Currently, 561 ACOs care for 10.5 million Medicare patients.
It sounds great, so what went wrong? Under the current law, there are three tracks of the ACO. The tracks are separated by risk level; Organizations that take on greater risk are rewarded with greater amount of the cost-savings they generate. Save more on health care costs—assuming care levels stay the same— and pocket more of those savings. Unfortunately, most ACOs function under the one-sided Track 1, in which they have more time to reap the benefits of the program by receiving a share of cost savings, but do not have to pay back their share of spending over the benchmark. As such, the CMS estimates that about 82% of ACOs do not take any risk for patient care, and are increasing Medicare costs.
In 2017, the most recent year data are available, about 60% of the 472 Medicare ACOs generated a total of $1.1 billion in savings for the CMS.
On December 21, 2018, the Centers for Medicare & Medicaid Services issued a final rule setting a new direction for the Medicare Shared Savings Program, referred to as “Pathways to Success.” This redesigns the participation options available under the program to encourage ACOs to transition to performance based risk more quickly and, for eligible ACOs, incrementally, to increase savings for the Trust Funds.
The CME believes that the benefits to taxpayers and Medicare recipients should have been realized after six years of the program, but this has not been the case. Under the new rule, CMS will reduce the three tracks to only two. New ACOs receive up to 25% of their savings over the first two years, but also have to assume risk by paying back a percentage of any losses.
As ACOs assume more risk, they are granted exemptions from federal laws, like the Stark laws that block physician self-referrals which are financially profitable.1,2 Even better, ACOs that take on higher risk patients and join the “Enhanced” track will get up to a whopping 75% of their savings under this new rule, according to CMS.
In an analysis, published Monday, May 6, 2019 in Health Affairs, it was found that the risk of an ACO leaving the Medicare program is cut by more than three-quarters if they receive shared savings for at least one performance year. Overall, 30% of the 624 ACOs that participated at some point in the first five years of the program left. The findings come a few months after the CMS overhauled the program, which will force ACOs to take on risk sooner. Since then, concerns have been raised about whether or not ACOs will join or stick with the program.
The rules have changed, so what now?
With the current trajectory, it is likely that up to 70% of the current ACOs will drop out of the program, saving taxpayers about $2.24 billion over 10 years.
However, what about the quality and coordinated care the program was supposed to achieve?
That may be on pause. Millions of beneficiaries will return to the uncoordinated, time-consuming and difficult-to-navigate maze that is Medicare health policy. So, while taxpayers might be saving money over the next ten years, are they saving time, energy and stress?
Interestingly enough, it appears that physician-led ACOs have had the most success of all ACOs. While the specific reasons for this are unclear, the physician-led model may be a way to salvage ACOs going forward. It is intriguing to think that we may have come back to where we started—a system in which physicians control their own practices and reimbursements. Maybe we had the right idea all along.
In a filing on May 2, 2019, Assistant Attorney General Joseph Hunt acknowledged that the administration had previously argued that parts of the law could remain in effect even if the individual (tax) mandate were struck down, but he said, the administration had come to believe it could no longer defend that position. He suggested that rewriting the statute by “picking and choosing which provisions to invalidate” would interfere with the role of Congress and the “proper course” for the courts would be to strike down the law in its entirety.
Now, the Trump administration is urging a conservative U.S. appeals court to cancel Medicaid coverage for 12 million Americans, insurance subsidies for 10 million more and the protections for 133 million people with preexisting conditions.
What’s the right answer? Does The Affordable Care Act work? Does it make sense? What’s the answer for an alternative?
References
- Ault, A ACOs failing to deliver, says CMS in issuing proposed overhaul. Aug 10, 2018. Medscape. Retrieved at: https://www.medscape.com/viewarticle/900551?src=wnl_edit_tpal&uac=137463DJ&impID=1709726&faf=1
- Center for Medicare & Medicaid Services. About the Program: Shared Savings Program. Mar 27, 2018. Retrieved at: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/about.html
- Center for Medicare & Medicaid Services. Medicare Program; Medicare Shared Savings Program; Accountable Care Organizations- Pathways to Success. Proposed Rule. Federal Register. Aug 17, 2018. Retrieved at: https://s3.amazonaws.com/public-inspection.federalregister.gov/2018-17101.pdf
- Gosfield A. The stark truth about the Stark law: part 1. Fam Pract Manage. 2003. Nov-Dec; 10(10):27-33.


