
Sometimes it may feel like there isn’t enough time in the day. Your projects are stretching you think as you try to balance work and home, too. You know you need help with the details, but delegating your to-do list to someone else may seem like another grueling step, an extra item on the to-do […]

It’s no secret finding the perfect job is a lot of work. Whether you’re fresh out of residency, or have been in the same job for years, deciding to take that leap and find your dream job is daunting and exhausting.
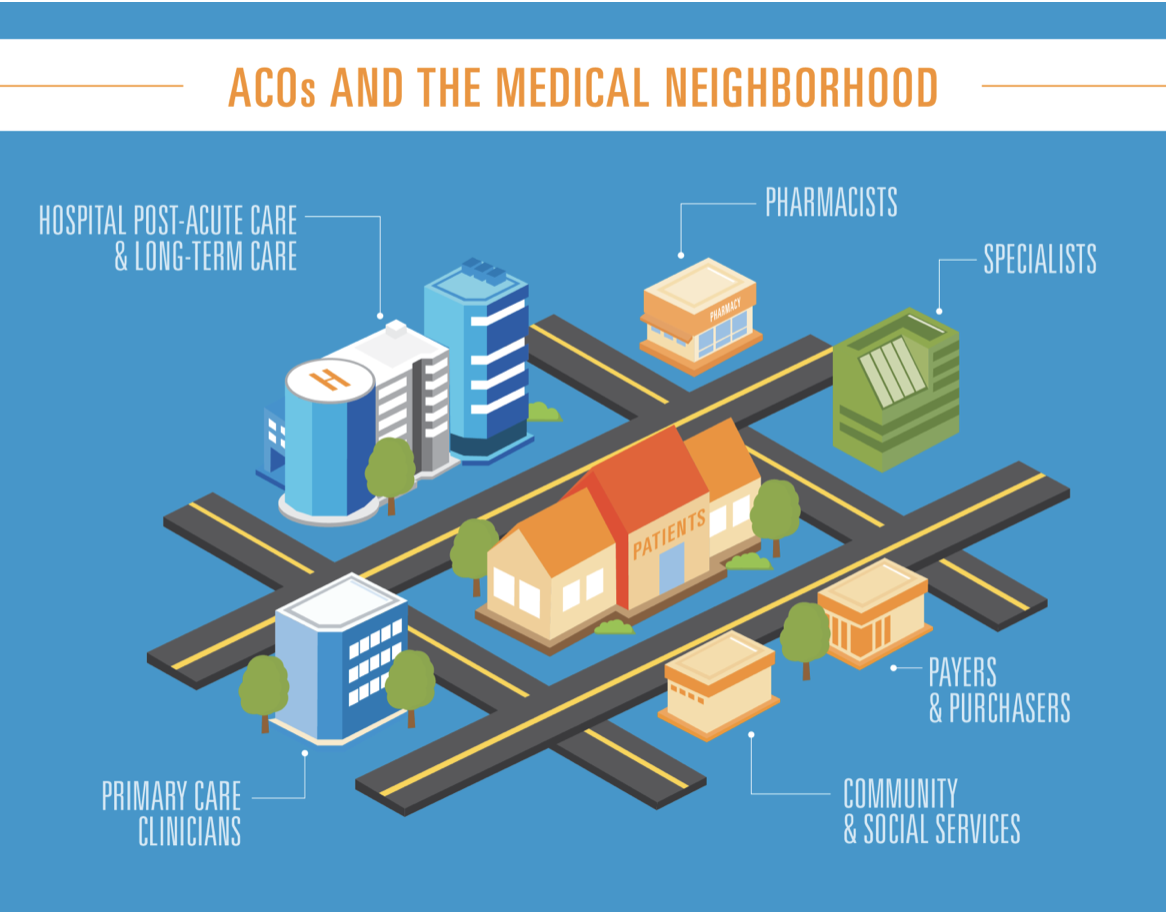
The Affordable Care Act (ACA) was meant to usher in a new era of healthcare, insuring millions more Americans and improving health care access. While the current state of The Affordable Care Act is still under scrutiny as it once again faces legal hurdles after President Donald Trump and his administration supported a lawsuit questioning the health-care law’s constitutionality, it’s important to ask the question, is it working?

While medicine remains a profession of lifelong learning and care of others, it is also very much a business. Physicians and other health care providers serve the needs of patients, but we can’t do so if we are unable to reach them. While a great number of physicians—apart from our pediatrician colleagues—focus their efforts on an aging patient base, the reality is that we may need to reconsider our marketing strategies. Millennials, the generation with an often obscure definition (sometimes born after 1983, sometimes as early as the late 1970s) is fast becoming a powerful market force. Made of around 1.8 billion adults, the group has now overcome the Baby Boomers as the largest generation, accounting for almost a quarter of the American population.
The notion of physician burnout has been discussed in quiet circles for decades, but it is being discussed even more frequently among medical professionals at large and even in lay publications.

Over 355,000 doctors in the United States are female. Throughout the United States, these doctors balance a variety of tasks: working 60 hour weeks, being a wife, caring for patients, working nights, maintaining a fitness routine, advocating for the needs of others, creating and changing policy, being an entrepreneur — and some do all of this while being a mother, too.

Maintaining a fitness routine while trying to keep up with a busy work schedule and taking care of your family can be near to impossible. For doctors, or those of us with a career in medicine, it can be particularly challenging. But, if being fit is a priority for you, you need to make time for it.

Talk about throwing down the gauntlet. In a provocative editorial published last year in Circulation: Cardiovascular Quality and Outcomes, Dr. John Ioannidis, who in 2005 shocked the scientific research community with his article “Why Most Published Research Findings Are False,” took aim at medical professional societies authoring clinical practice guidelines and disease definition statements. He observed that despite notable progress in improving the trustworthiness of guidelines since the 2011 Institute of Medicine report Clinical Practice Guidelines We Can Trust, guideline panels continue to be plagued by financial conflicts of interest, lack of methodologist involvement, and domination by specialists “who have overt preferences (even without overt conflicts).”

Every business, whether big or small, new or developed, can benefit from cutting every day costs. And a little money saved every day goes a long way. For medical practices, trimming some of these daily expenses means more money and time can go into the care and support of patients. At the end of the day, isn’t that what all physicians want?

In business, nothing is more important than your reputation. It can positively sustain and grow a patient base or destroy it. Simply put: a positive reputation leads to an increase in patients that walk through your door.

While doctor depression and suicide rates continue to climb to record highs, the term “burnout” has also increased in popularity. There is an ongoing debate on whether to refer to this systemic exhaustion as burnout, doctor disempowerment, moral injury, or human rights violations. Semantics aside, healthcare providers across the U.S. feel “overwhelmed, demoralized, exhausted, cynical, afraid, and alone”. The industry has put it in doctors’ hands to balance 20 hour shifts, patient care, online reputations, continued education, teaching, charting, administrative duties, technology, and community outreach — as if being a physician is a typical 40-hour work week. At the same time, many doctors balance their 80-hour a week job while being entrepreneurs, business owners, spouses, parents, or students and managing physical and mental wellness. Coping with the ever heightened standards of the medical profession is no easy task.

There is an opioid crisis in America and our patients are aware of it. Did you know that 530 individuals die each week due to opioid overdose.1 The media has effectively publicized this growing problem, and patients are aware of the role that legally prescribed opioid medications can play in dependence and addiction. Congress and state governments are also paying attention.
In February 2018, Congress promised $6 billion over two years for initiatives to fight opioid abuse, and many state legislatures have proposed limitations to the number of opioid pills physicians can legally provide to their patients. Right or wrong, physicians must be aware of these new laws and be willing to change their prescribing practices in order to comply. However, instead of waiting for legislation to shape our practices, we can and we should look to new guidelines to help patients avoid developing dependence on prescription opioids in the first place.